Synthetic Peptides vs. Recombinant Peptides: Choosing the Right Path for Your Drug
The choice between synthetic and recombinant peptides is no mere fork in the road; it’s the GPS guiding your drug development journey. Both paths offer unique opportunities, but understanding their nuances ensures your drug doesn’t take a wrong turn.
Synthetic peptides are the chemist’s masterpiece—produced entirely in a lab. Their precision allows for custom modifications, making them ideal for short sequences or specific functionalities. Need an exotic amino acid? Synthetic peptides deliver it on a silver platter. Plus, they’re cost-effective for small-scale production, especially in the early research phases. However, as sequence length increases, so does complexity, often hitting a scalability ceiling.
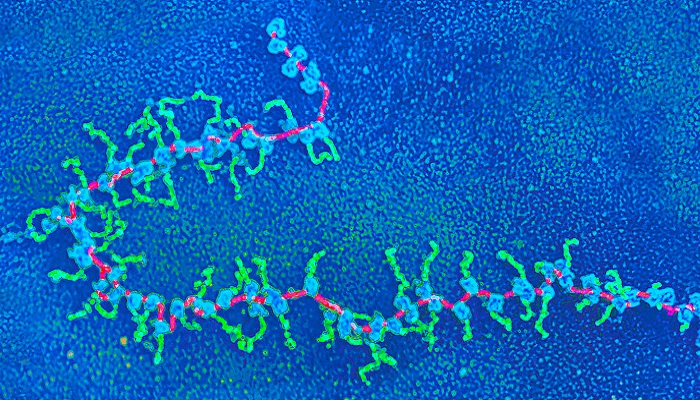
Enter recombinant peptides, nature’s handiwork harnessed through biotechnology. Produced using living cells, they excel in creating longer, more complex sequences with post-translational modifications. Think glycosylation or phosphorylation—the details synthetic methods struggle to replicate. They’re your go-to for biologics requiring high fidelity and natural structure. The catch? Initial setup is costlier and time-consuming, akin to planting a tree—slow to grow but rewarding in the long run.
Imagine this: A biotech team debates options for a cancer therapy peptide. One scientist argues for synthetic peptides, citing rapid development needs. Another favors recombinant for its scalability. The compromise? Start synthetic for preclinical studies, then transition to recombinant for clinical manufacturing.
So, how do you choose? Consider factors like sequence complexity, scale, and cost. Synthetic is the sprinter; recombinant is the marathoner. Each has a role, but success depends on aligning the choice with your drug’s unique roadmap.
The stakes are high, but the rewards—life-saving therapies—make it worth the trek. Will your drug's journey be a sprint, a marathon, or both?